Depressionomics? Win for mental health investments
Investing in mental health care will pay off for the Australian economy, write Australian Medical Association President Steve Robson and Australian National University Associate Professor Jeffrey Looi.
Just over two years ago, the Australian Productivity Commission’s report into mental health was released to the public.
The report had been instigated by then federal Treasurer Josh Frydenberg, giving terms of reference directing the Commission to: “consider the role of mental health in supporting economic participation, enhancing productivity and economic growth. It should make recommendations, as necessary, to improve population mental health, so as to realise economic and social participation and productivity benefits over the long term.”
Implicit in the task, then, was the fact that mental health has an important effect on the economy and that community-wide improvement in mental health had the potential to benefit everyone — whether they have mental health problems or not — through an improved economy.
How do mental health issues affect the economy?
Estimating the effect of mental health conditions across the community — beyond the direct costs of diagnosing and managing individuals — presents challenges.
There are three common approaches to making this type of economic estimate: the human capital approach, the economic growth approach, and the value of statistical life approach. Such analyses aim to account not only for the hidden costs of mental health conditions, but on broader effects on the economy as a whole.
Studies that have used these approaches estimate that the broader costs to the economy of mental health conditions dwarf the direct costs of treating the disease for the individual. The Productivity Commission report calculated the cost to the Australian economy of between $40 billion and $70 billion each year.
Systematic reviews of the direct and indirect costs of mental health conditions at a global level paint a picture confirming the economic burden of common mental health conditions.

How can mental health problems have such an enormous effect on the economy?
Beyond the direct costs of providing care to individual patients, people affected by chronic or severe mental health conditions are less likely to work in higher paid jobs, or to work at all. This means that they buy fewer things, pay less tax, take fewer holidays or travel, and spend less into the economy. They are also more likely to require financial assistance to live their lives, such as through social security benefits and the National Disability Insurance Scheme.
Providing care for people with mental health conditions has an obvious human benefit. Mental health conditions can cause great distress and debility for those affected, and for family and friends who love and care for them. There are overwhelming compassionate reasons to treat mental health conditions to help alleviate suffering. Yet for those who are not directly involved and who take an economic approach, providing effective treatment for mental health conditions makes good sense.
Mental health conditions are common
Data from the Australian Institute of Health and Welfare (AIHW) reveal that as many as one in five Australians will have had a mental health condition each year. Fortunately, most of these conditions will be relatively mild and self-limiting. However, close to 800 000 people will have a severe mental illness. To put these figures in perspective, mental health conditions represent about 13% of the total burden of disease in Australia, behind only cancer, musculoskeletal conditions and cardiovascular diseases.
Although it is difficult to make accurate assessments, data from the AIHW confirm that the coronavirus disease 2019 (COVID-19) pandemic has increased the burden of mental health conditions across the Australian community. This trend is global and, importantly, pandemic measures such as lockdowns have been found to have a disproportionate effect on women and those at disadvantage.
Since the ongoing COVID-19 pandemic has had adverse effects both on the fiscal position of the government and the mental health of people in the community, it would seem prudent to improve treatment of those with mental health conditions not only to make lives better for those directly affected but as a way of boosting the government financial position overall. So, if we are going to accomplish this, and spend money on addressing mental health needs, where is expenditure most likely to have an effect?
Three key innovations for a sustainable mental health care system that
meets the needs of Australians
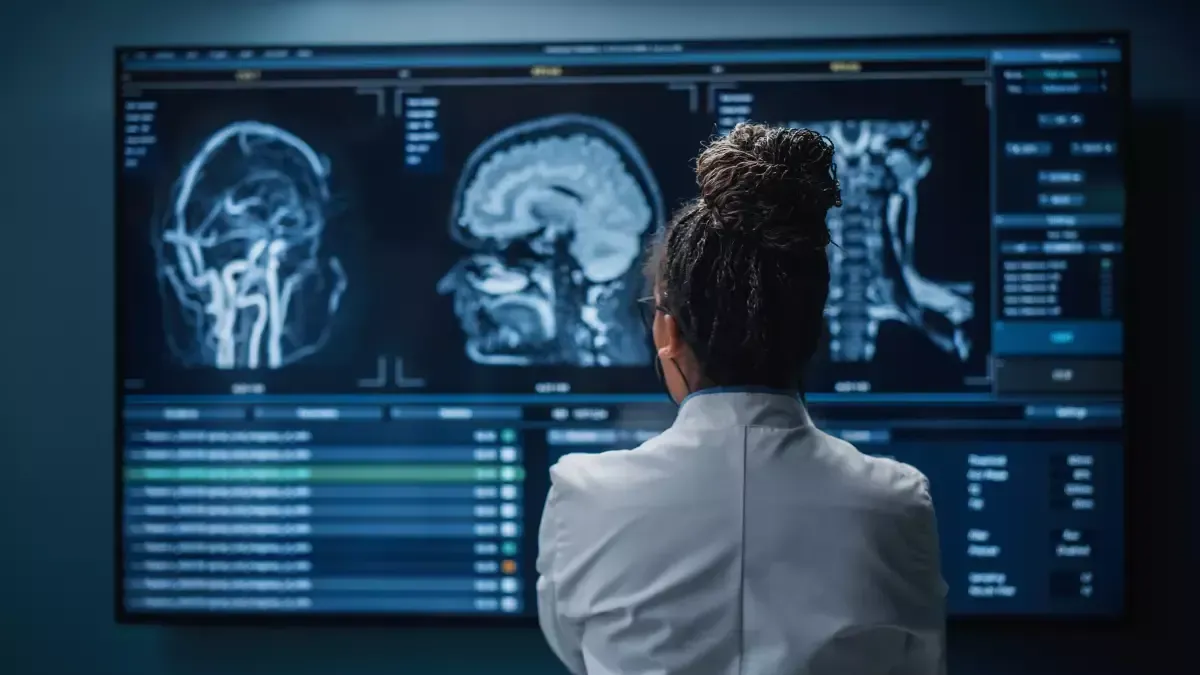
There is a need to address the burden of disease measured as years of life lost to disease and injury (ie, disability-adjusted life years), and the five chronic disease groups that are the main burden identified by the AIHW in 2022 were cancer (17%), musculoskeletal conditions (13%), cardiovascular diseases (12%), mental health conditions and substance use disorders (12%) and neurological conditions (8%).
Of the individual diseases, the leading burdens were from coronary heart disease (5.5%), dementia (4.4%), back pain and problems (4.2%), chronic obstructive pulmonary disease (3.7%) and anxiety disorders (2.9%). Due to the pandemic, there was a considerable burden because of COVID-19.
Across the lifespan, there is prominence of the burden of mental health and substance misuse conditions, especially in children (five to 14 years), youth (15–24 years) and mature adults (25–44 years), with anxiety disorders ranked first or second for females, and anxiety and suicide or self-related injuries ranked first or second for males in these age ranges. For older men and women (aged over 65 years), dementia is first or second.
Matching the initiatives to these needs requires strengthening and innovation for mental health care, founded on several key innovations. First, there is an urgent need to reinstate the federal and state funding of acute hospital services. By clearing the hospital logjam, the capacity to improve the emergency department flow and bed access should increase, improving the experience of acute mental health care for patients with mental health conditions and substance use disorders. Currently, patients with severe illness experience difficulty accessing emergency care and inpatient treatment. Improvements in acute hospital care will also flow through to enhance the effectiveness of public community mental health care.
Second, suicide not only has an extraordinary effect on Australians but is estimated to cost the Australian economy close to $2 billion each year. The prevention of suicide remains an enormous challenge, although economic and social supports have been demonstrated as important factors, and improving the quality of acute hospital and community care will underpin emergency responses.
Third, modernising Medicare around general practice by innovation in the co-location of allied health staff, such as psychologists, occupational therapists and social workers, and streamlining shared care with psychiatrists in public and private sectors, through specific purpose-built liaison services hosted in general practice and public sector services, will enhance early intervention at the point of first consultation in general practice.
In exactly the same way, there should be targeted initiatives to diagnose and treat anxiety disorders in youth and mature adults through general practice that is supported with access to specialised psychological therapy for anxiety and related disorders, including by psychologists, psychiatrists and allied health professionals in shared care.
Lastly, providing general practice-led multidisciplinary care for people with dementia is necessary to address both their physical and mental health needs. GPs will need support in relation to diagnostic assessment, treatment planning, and ongoing consultative advice on management of complications of dementia (behavioural and psychological symptoms etc) from geriatric medicine, old age psychiatry and other specialised in-reach support services for outpatient, community and residential aged care facilities.
Similarly, strengthening the private health care system by preserving patient and doctor choice of treatment and venue of care will complementarily support public mental health services, as private services provide the majority of inpatient care for severe anxiety and mood conditions and substance misuse disorders.
There has been relative stasis of public hospital bed numbers across all Australian states, while there has been a relative increase in private hospital bed over time. Therefore, if there is not an increase for beds overall, as a result of expansion in the private sector, psychiatric bed capacity overall declines and remains below international benchmarks for the number of beds per 100 000 population for high income countries. This can contribute to hospital access blocks, as there are short lengths of stay that may potentially mitigate against full recovery for safe discharge of patients to follow-up community care.
As things stand, mental health conditions — both acute and chronic — have an enormous impact on the Australian economy. Government investment in evidence-based targeted programs has the potential to deliver a significant economic payoff at a time when governments at all levels are facing major funding challenges.
The evidence is already pointing us in the right direction — 2023 should be the time for action.
Recent Posts