Will the pandemic have an effect on men’s fertility in the long term?
Although it is always difficult to provide an exact figure, the proportion of couples who experience a fertility delay is likely to be high.
Recent, pre-pandemic, estimates suggest that as many as one in nine couples will experience infertility. It is also commonly reported that men’s fertility issues contribute to about half of all diagnoses of infertility. These findings are not confined to high-income countries - male infertility is recognized as a health issue globally.
Although the evidence initially was contentious, recent reviews have confirmed that there has been
a gradual decline in semen parameters globally over the last few decades. While a sperm concentration of about 15 million/mL is accepted as the lower limit of normal in a semen analysis, there is good evidence that the
fertility potential of sperm begins to fall with concentrations well about this level.
The pandemic initially saw
a significant reduction in birth rates across the world. While there has been some evidence of a ‘baby bounce’ after the first wave of the pandemic,
the longer term trend is fertility is gloomy with birth rates dropping across the world.
Before the pandemic it was clear that the use of technologies such as IVF was increasing, with a
major trend to IVF conception in countries like Australia. Are there reasons to be concerned that the COVID-19 pandemic could affect the family plans of Australians?
In the first instance, there has been a large amount of anti-vaccine propaganda circulated on social media. It can be difficult for people without scientific training to understand and interpret
mis- and disinformation that crops up in their social media feeds. Fortunately, the news about COVID-19 vaccination and Systematic reviews have been unequivocal – there is
no adverse effect of vaccination against COVID-19 on men’s fertility. That is very reassuring news.
The information we have about COVID-19 infection and men’s fertility is not so good, however - I’d like to run you through that
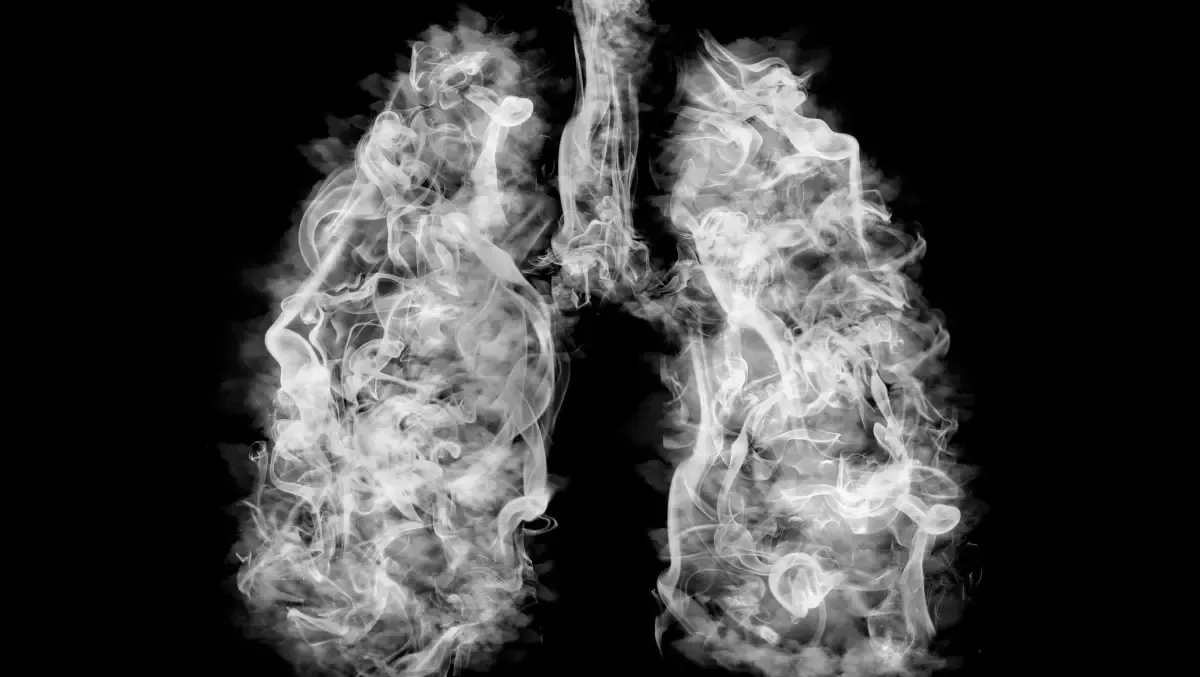
The COVID-19 virus enters human cells by
interacting with angiotension converting enzyme 2 (ACE-2) receptors. Cells that express the ACE2 receptors are very vulnerable to infection with the virus. There are a number of
cells, organs, and tissues – including the lungs and blood vessels – that carry high numbers of receptors.
The hormones that control and regulate sperm production in men originate in the hypothalamus and anterior pituitary gland. COVID infection has been identified in the
pituitary gland and hypothalamus. It shouldn’t be surprising, then, to find that men recovering from infection have
alterations in pituitary hormones such as luteinizing hormone (LH) and the hormone LH stimulates production of – testosterone.
While there is the potential for COVID infection to cause transient changes in a man’s hormonal status, is there any evidence for more direct effects on fertility?
Well, yes.
Studies suggest that sperm parameters in men who have recovered from COVID infection are lower than men who were not infected. Indeed,
in studies in which testicular tissue could be examined, investigators have found that coronaviruses are associated with inflammation of the sperm-manufacturing cells in the testes – a situation that has potential for long-term damage. This is the mechanism by which
mumps can cause sterility in men.
It seems that we have evidence that COVID infection involves the glandular and hormonal controls of sperm production and fertility in men. We also have direct evidence that the virus infects the testes – indeed, the testes have been found to have
high levels of ACE2 receptors.
How could we tell if the pandemic was affecting men’s fertility? It is a notoriously difficult question to answer – being able to discern people’s intentions obviously is impossible. However, we can find clues if we know where to look.
One possible example is the uptake of sperm testing. If men’s fertility was being affected across the population, then we would expect to see a greater number of couples seeking evaluation for infertility. The primary test of male fertility is the
semen analysis. On possible signal that male fertility problems are resulting from COVID infection at a population level would be a persistent rise in the number of sperm tests being performed around the country.
The hypothesis that fertility problems are more common since the pandemic – and have resulted in a greater need to perform sperm tests – is easy to test. Virtually all diagnostic sperm tests performed in Australia are billed through Medicare. It is possible to monitor Medicare billing in close to real time by searching the
Services Australia website.
I have downloaded data from the main Australian states – and excluded Western Australia as the hard border protected the population from the pandemic for a long time – to assess the number of sperm tests performed prior to, during, and after the acute medical disruptions of major waves. Interestingly, and discounting the disruption caused during lockdowns and the major initial pre-vaccination waves, the raw number of sperm tests performed since the start of 2022 is higher that the pre-pandemic period, and shows a steeper upward trend.
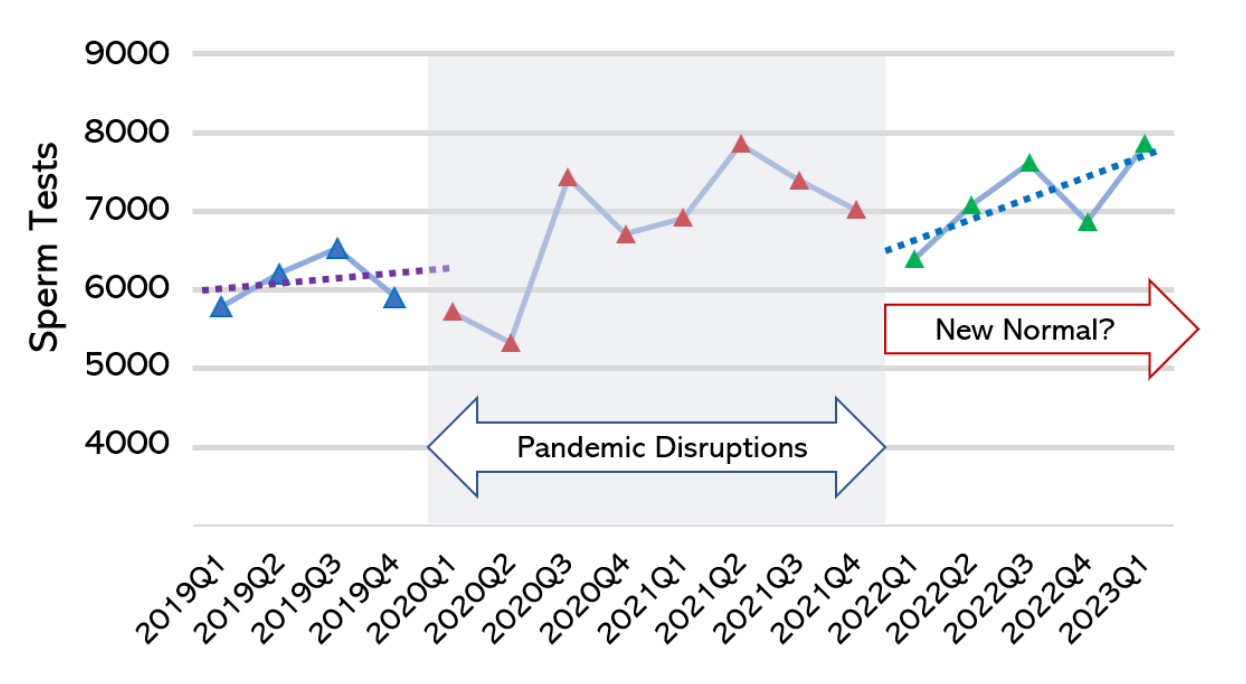
These are early days and Medicare billing data are, at best, a crude way of looking at a complex clinical phenomenon. However, there is enough of a signal in these data to suggest that we need to watch closely. In particular, while a man who had healthy sperm production is very unlikely to have been rendered infertility by COVID infection, there are many men with borderline sperm parameters. The physiological insult of COVID infection and its selective effect on sperm production could potentially be enough to tip that man into true physiological infertility.
It may well take several years to form a true and interpretable picture of the effect of the pandemic on the men of Australia and their fertility. However, it seems that we have a physiological basis to be concerned and there already is a signal in the data that is consistent with a population-wide effect on men’s fertility.
I will be watching very closely.
Recent Posts