Migration and its implications for health services
THE emergence of modern Australia is a story of immigration. The peaceful settlement of millions of post-war migrants has been one of Australia’s greatest achievements and has been a key driver of our economic and social development.
Of the 19 million Australians aged 15 years and older who live here now, almost seven million were born overseas. Indeed, about 28% of Australia’s overall population was born overseas, among high income countries a proportion only exceeded by Luxembourg and Switzerland.
As a migration nation, the structure and shape of the Australian economy has formed around the constant flow of managed immigration. Australia’s growth rate, labour force capacity, and innovation capabilities all assume the continuation of a robust migration regime. For almost 30 years, Australia’s economy has had about a 3.0% rate of compound annual growth: in the absence of the additional population growth of 1.4% per year, the economy would only have grown at about 1.6% each year in per capita terms. Looking forward, it is estimated that Australia’s migration program will contribute $1.6 trillion to the Australian economy by 2050, making the continuation of a significant migration program an economic, if not political, imperative.
Annual population increases within Australia comprise births and incoming migration (“net overseas migration”) — the relative values for the year 2015 are shown in Figure 1.
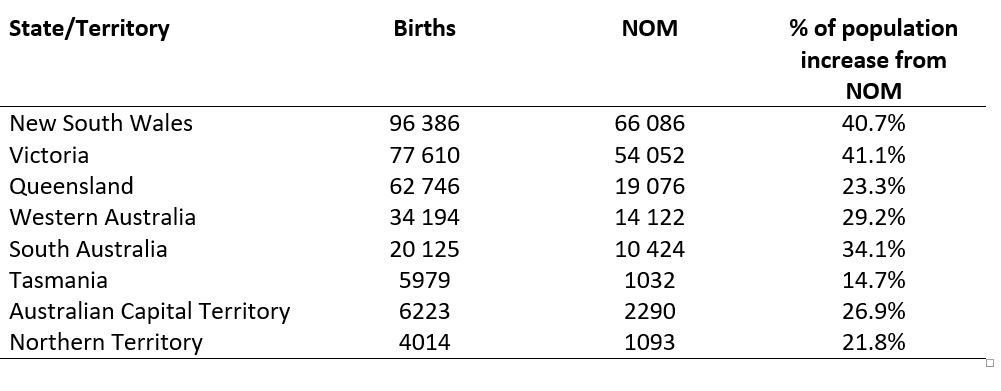
As the population expands, increased demands are placed on infrastructure, housing, and essential services, of which health is a major component. For a child born in Australia, there exists a relatively predictable trajectory of health needs; however, things are not so clear for migrants arriving in Australia.
Since the abolition of the White Australia Policy, our immigration program has been framed around a set of core principles, operating in accordance with Australia’s national interests and values (Figure 2).
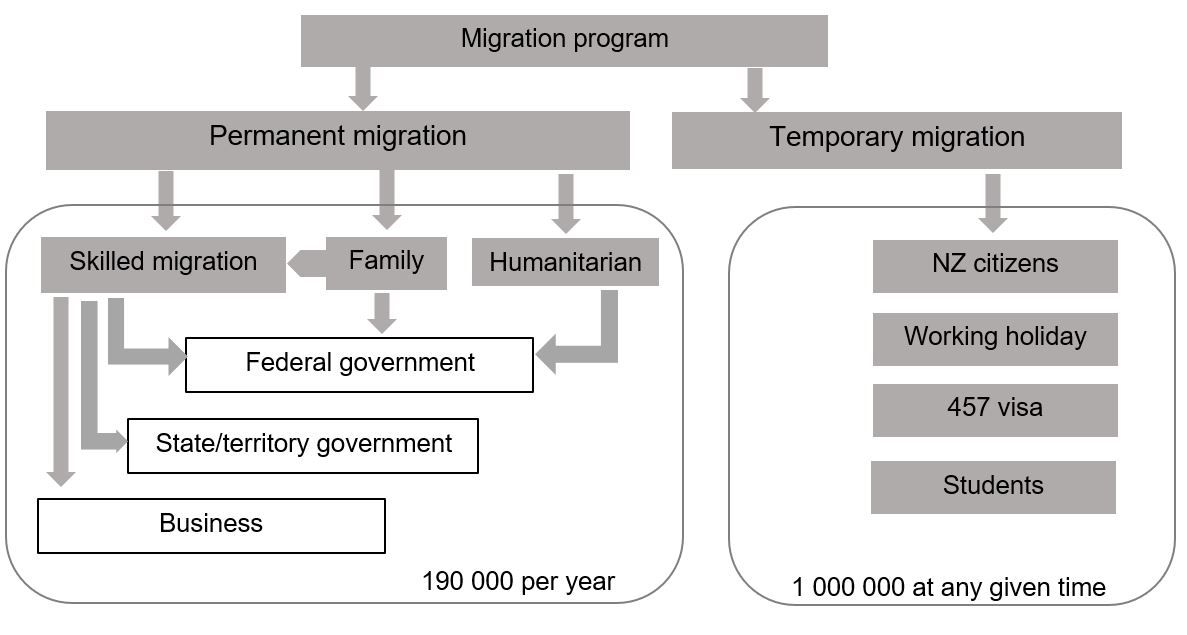
The program is non-discriminatory and while it may select for skill sets and language level, selection is irrespective of country or origin, religion, gender or ethnicity. Further, the framework favours permanency and citizenship and has a strong emphasis on family reunion and on family units, enabling skilled visa applicants to be accompanied by their spouse and dependent children. Finally, Australia has made an ongoing commitment to a humanitarian program selected through the United Nations High Commissioner for Refugees (UNHCR), with referrals based on need and vulnerability. In addition, historically relatively generous medical waivers were given to those referred.
The characteristics of our migration system have meant that in the past 30 years, our program has seen the settlement of new arrivals from every corner of the globe and from almost every linguistic and cultural group around the world. This diversity has been a source of national strength, but also requires strategic planning and foresight in the design of our institutions and our systems, particularly those that interface with newly arrived Australians when they are at their most vulnerable. One important interface is the health system.
Australia has a universal health system through Medicare and its medical benefit and pharmaceutical benefit schemes. For universal health care to function, patients must be equipped to access, understand and participate in the system. While some migrant groups will find Australia’s health system familiar to that of their pre-migrant experience, our health systems will be difficult to navigate for many migrants, necessitating a level of assistance to allow equitable access. Barriers to access can have important implications for provision of health care. For example, primary care may be neglected, allowing conditions to go untreated until more serious — migrants are less likely to participate in screening programs or to access vaccination services.
The “healthy migrant effect”
Migrants who come to Australia through skilled migrant programs typically have to meet health standards, thus they tend to have a higher standard of health at arrival than the general Australian population: this is known as the “healthy migrant effect”. However, there is evidence that, once in Australia, this level of health tends to deteriorate. For most migrants, no access to Medicare is permitted for the first 104 weeks after arrival, and this presents another barrier to health care access. At the time of writing, there is a current proposal to increase this waiting period further.
After arrival, migrant groups experience disproportionate disease burden, depending on their ethnicity and pre-migration health status, and increased health care utilisation has been found among migrant populations in Australia. Although older studies have reported that migrants tend to have lower rates of hospital surgical admission than patients born in Australia, overall hospital admissions, emergency department presentations and admissions due to potentially preventable infectious diseases are above the Australian-born averages. Hospital admission rates for vaccine-preventable illnesses are approximately 20% higher in migrants, and rates of admission for diabetes, coronary artery disease and other chronic heart disease may be up to 50% higher.
Many migrants to Australia will face an adverse impact on their health resulting from low English proficiency, or circumstances and considerations relating to their ethnicity and cultural or religious beliefs. The impact of this on primary care in community settings is difficult if not impossible to measure and only marginally less difficult to quantify for hospital-based services. Studies suggest that the cost per weighted activity unit of migrant patients is greater than Australian-born patients.
As a simple example one large study reported that, according to demographics of the areas that hospitals serve, the cost of interpreters varies as an overall overhead from 0.3% to 5.8% in different areas. The same study found that non-English speaking (“culturally and linguistically diverse” – assessed by requirement for an interpreter or preferred language not being English) patients spend longer in hospital in the same diagnostic-related group (DRG), and that they incur higher average ward nursing and ward medical costs by DRG. Importantly, there is also a shift in severity towards more severe adjacent DRGs, suggesting that non-English speaking patients tend to have a higher proportion of comorbidities and complications. Overall, linguistic diversity was associated with a higher cost per weighted activity, ranging from 0.2% to 3.8%. Non-admitted episodes of care, typically to emergency department attendances, also incur a higher cost due to a greater proportion of triage category one presentations and a trend to older age.
The importance of planning
Providing adequate health services for migrants is fundamental: international human rights agreements enshrine the principle that all individuals have “rights to health and to a standard of living adequate for health”. When actions, overt or inadvertent, inhibit certain groups’ access to health care, this fosters a sense of “exclusion, social illegitimacy, and separation from the moral community,” with ramifications beyond the health inequities alone. Vissandjee and colleagues frame it thus:
“For … migrant cohorts whose previous life experiences incorporate vastly different cultural mores and modes of health care practice … [advancing migrant health to assist in] overcoming barriers to accessing care goes far beyond developing language comprehension and an individual’s ability to schedule an appointment.”
Public hospitals in Australia are under pressure to meet the demands of a growing population. Public hospitals are almost entirely the responsibility of state and territory governments — provision of health services comprises the single largest item in all state and territory budgets. The commissioning of new health infrastructure, resources and staffing to cater for community needs has a long lead time so it needs careful planning. However, while planning has focused on aggregate population movements, less attention has been given to the changing characteristics of Australia’s population and the need to manage access barriers for populations with significant language and cultural obstacles to equality of care.
Migration offers Australia enormous social and economic benefits, but responsible policy requires planning around the flow-on effects of a robust migration level. Sixty per cent of Australia’s future population growth is likely to flow from migration. Some 85% of migrants live in urban areas and this pattern is likely to continue. Migration is a national policy that finds its effect on local communities and has an impact on state and territory services. The windfall of migration is a net positive on the budget bottom line and strong gross domestic product growth. However, this economic boon needs to be matched by well coordinated services and systems which are responsive to a changing need.
The unique health considerations pertaining to migrants challenge our health systems, and this in turn places strain on the resources available to provide care to entire communities. We believe that, in the same way that roads and housing must be planned, it is time for greater coordination and investment to enable adequate health infrastructure and resources to be planned and delivered. Indeed, this needs to be a priority for Australia if we are to provide the fundamental services necessary. Health is fundamental to almost everything else.
Recent Posts